Overview
The demand for home and community-based care will grow as more elderly populations prefer to age at home. Even with the growth, home healthcare providers will continue to face significant headwinds. The labor shortage will continue to be a considerable challenge. In addition, labor shortage, wage growth, and inflation will pose additional challenges for home care agencies. Reimbursement cuts and other regulatory requirements will also pressure agencies' bottom line.
Effective Revenue Cycle Management will improve cash flow and enable home care agencies to meet the ongoing challenges. Contrary to the perception that Revenue Cycle Management starts after billing, it begins at intake and continues through authorization, scheduling, billing, and collections.
Effective Intake Process plays an outsized role in Revenue Cycle Management. Collecting timely and accurate information at the point of referral and intake will help Home Care Agencies to reduce denied claims and improve reimbursement time and cash flow. Home Care Agencies must leverage technology and integrated intelligent automation to improve intake efficiency and enable their staff to do more with less. Improving cash flow will help agencies continue providing quality care and improve patient and employee satisfaction.
In this blog, we will discuss some of the critical features of Home Care software to improve the Intake process and Revenue Cycle Management.
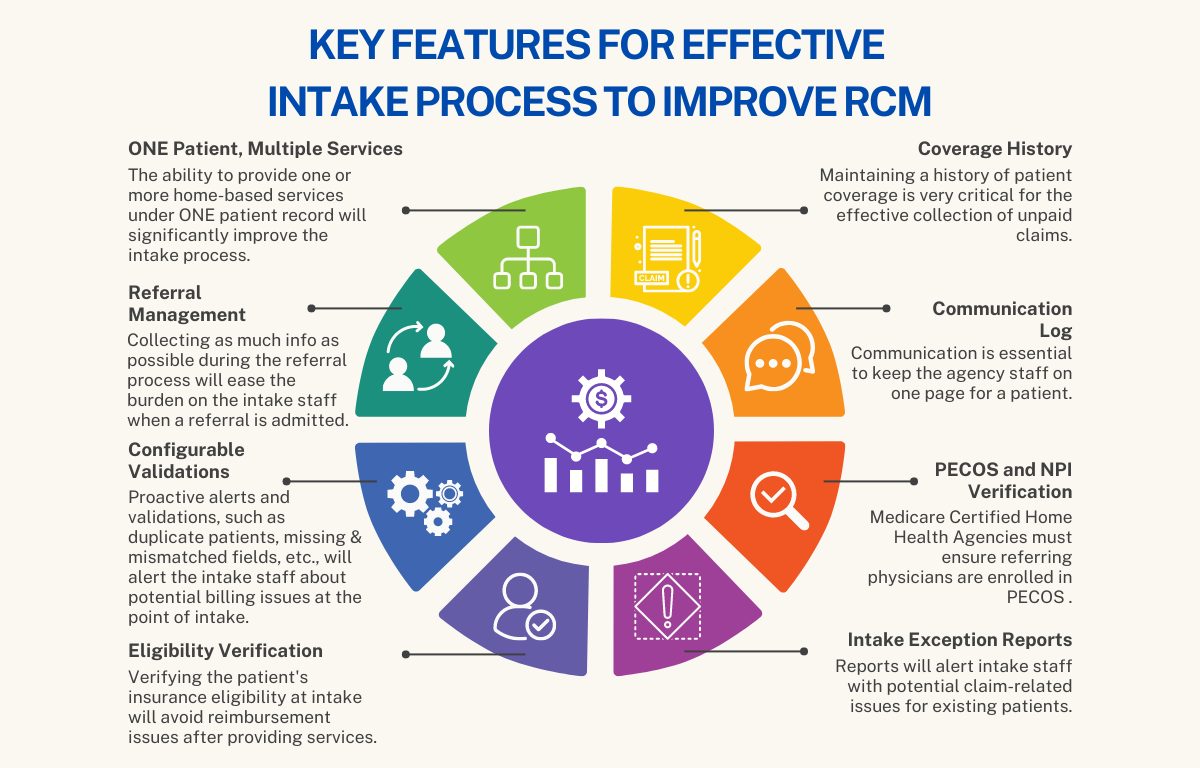
Key Features for Effective Intake Process to Improve RCM
Home Care Agencies, especially Private Duty Nursing and Non-Medical agencies, face unique challenges in meeting disparate, complex, and constantly changing billing requirements.
The following are some key software features that will help home care agencies improve their intake process.
ONE Patient, Multiple Services
The ability to provide one or more home-based services under ONE patient record will significantly improve the intake process for a home care agency. Keeping one patient record for all services will eliminate duplicate data entry and reduce errors and inconsistencies between multiple records for the same patient. A consolidated view of financial records will improve billing and collections for all services.
Referral Management
Collecting as much information as possible during the referral process will ease the burden on the intake staff when a referral is admitted for care. Converting a referral to an admission should retain all the information collected during the referral process.
Configurable Validations
Proactive alerts and validations, such as duplicate patients, missing fields, mismatched fields, etc., will alert the intake staff about potential billing issues at the point of intake. Home Care software should allow the agencies to configure the validations based on their needs. It will also be beneficial if the software enables the agencies to make fields required based on their process. Proactively detecting and notifying potential claim issues at intake will improve clean claims, reduce denials, and improve cash flow.
Eligibility Verification
Verifying the patient's insurance eligibility at intake will avoid reimbursement issues after providing services. Eligibility Verification is more than just a one-and-done task. Home care agencies should verify eligibility regularly to capture any lapse or change in patient coverage. Right home care software platform should provide multiple choices for eligibility verification – Real-Time, Batch, or Scheduled. Automating eligibility verification and notification will improve the efficiency of the intake process and revenue cycle management.
Coverage History
Patients usually change coverage periodically from one payer to another. Changing payers has become more frequent with Medicare Advantage and Medicaid Managed Care. Maintaining a history of patient coverage is very critical for the effective collection of unpaid claims. Home Care Software should have a mechanism to record all payers for the patient.
Communication Log
Communication is essential to keep the agency staff on one page for a patient. Home Care Software should be able to keep all communication in one place that is easily accessible to all users based on their roles.
PECOS and NPI Verification
Medicare Certified Home Health Agencies must ensure referring physicians are enrolled in PECOS (Provider, Enrollment, Chain, and Ownership System) as Medicare Providers. Home Care Software should have an integrated option to verify PECOS enrollment at the time of intake and regularly.
Intake Exception Reports
Home Care Software should have intake exception reports to run on a recurring schedule and send the results to selected users. These reports will alert intake staff with potential claim-related issues for existing patients.
Conclusion
Home Care Agencies should look for a software platform with functions and features to make the intake process efficient. Revenue Cycle Management starts at intake, and an effective intake process will improve collections and cash flow. CareVoyant Home Care software platform offers the right technology and tools to help home care agencies to improve intake efficiency, cash flow, and the bottom line.
ABOUT CAREVOYANT
CareVoyant is a leading provider of cloud-based integrated enterprise-scale home health care software that can support all home-based services under ONE Software, ONE Patient, and ONE Employee, making it a Single System of Record. We support all home based services, including Home Care, Private Duty Nursing, Private Duty Non-Medical, Home and Community Based Services (HCBS), Home Health, Pediatric Home Care, and Outpatient Therapy at Home.
CareVoyant functions – Intake, Authorization Management, Scheduling, Clinical with Mobile options, eMAR/eTAR, Electronic Visit Verification (EVV), Billing/AR, Secure Messaging, Notification, Reporting, and Dashboards – streamline workflow, meet regulatory requirements, improve quality of care, optimize reimbursement, improve operational efficiency and agency bottom line.
For more information, please visit CareVoyant.com or call us at 1-888-463-6797.
Request for Information
To learn more about CareVoyant Software and how we improve the operational efficiency of Home Healthcare Agencies, contact us: