What are Home and Community Based Services?
Millions of Americans, including children, adults, and seniors, need long-term care services because of disabling conditions and chronic illnesses. Medicaid is the primary payer across the nation for long-term care services. Medicaid allows for the coverage of these services through several vehicles and over a continuum of settings, ranging from institutional care to community-based long-term services and supports (LTSS). Two significant components of LTSS are Institutional services and Home and Community Based Services (HCBS).
Home and Community-Based Services (HCBS) are person-centered care delivered in the home and community. HCBS programs address the needs of people with functional limitations who need assistance with everyday activities, like getting dressed or bathing. HCBS are often designed to enable people to stay in their homes rather than move to a facility for care.
Home and Community-Based Services (HCBS) allow Medicaid beneficiaries to receive services in their home or community rather than institutions or other isolated settings. These programs serve a variety of targeted population groups, such as people with intellectual or developmental disabilities, physical disabilities, or mental illnesses. Over 3.5 million individuals receive HCBS through various Medicaid Waiver programs.
History and Options:
Home and Community-Based Services (HCBS) first became available in 1983 when Congress added section 1915© to the Social Security Act, giving states the option to receive a waiver of Medicaid rules governing institutional care. In 2005, HCBS became a formal Medicaid State plan option. Several States include HCBS services in their Medicaid State plans. Forty-seven states and DC are operating at least one 1915© waiver.
State Medicaid agencies have the following four HCBS options:
1915© - Home and Community-Based Waivers
Within broad Federal guidelines, States can develop home and community-based services waivers (HCBS Waivers) to meet the needs of people who prefer long-term care services and supports in their home or community rather than in an institutional setting.
Nearly all states and D.C. offer services through HCBS Waivers. States can operate as many HCBS Waivers as they want — currently, more than 300 HCBS Waiver programs are active nationwide.
State HCBS Waiver programs must:
Demonstrate that providing waiver services won’t cost more than providing these services in an institution
Ensure the protection of people’s health and welfare
Provide adequate and reasonable provider standards to meet the needs of the target population
Ensure that services follow an individualized and person-centered plan of care
1915(i) - State Plan Home and Community-Based Services
States can offer services under a State Plan Home and Community Based Services (HCBS) benefit. People must meet state-defined criteria based on need and typically get a combination of acute-care medical services (like dental services and skilled nursing services) and long-term services (like respite, case management, supported employment, and environmental modifications) in home and community-based settings.
1915(j) - Self-Directed Personal Assistance Services Under State Plan
Self-directed personal assistance services (PAS) are personal care and related services provided under the Medicaid State plan or section 1915(c) waivers the State already has in place.
Participation in self-directed PAS is voluntary
Participants set their own provider qualifications and train their PAS providers. Participants determine how much they pay for a service, support, or item
1915(j) State Options
States can:
Target people already getting section 1915© waiver services
Limit the number of people who will self-direct their PAS
Limit the self-direction option to some regions of the State, or offer it Statewide
At the States option, people enrolled in 1915(j) can:
Hire legally liable relatives (such as parents or spouses)
Manage a cash disbursement
Purchase goods, supports, services, or supplies that increase their independence or substitute for human help (to the extent they’d otherwise have to pay for human help)
Use a discretionary amount of their budget to purchase items not otherwise listed in the budget or reserved for permissible purchases
1915(j) Person-Centered and Directed Planning Process
Service plan is based on an assessment of the need for PAS
Service plan and budget plan are developed using a person-centered and directed process
Participants can engage in and direct the process
Participants can choose family, friends, and professionals to be involved as needed/wanted
Participants’ preferences, choices, and abilities, as well as strategies to address these preferences must be identified in the service plan
The plan must include an assessment of contingencies that pose a risk of harm to participants and an “individualized backup plan” to address those contingencies, as well as a “risk management plan” that outlines risks participants are willing to assume.
1915(k) Community First Choice
The “Community First Choice Option” allows States to provide home and community-based attendant services and supports to eligible Medicaid enrollees under their State Plan. This State plan option was established under the Affordable Care Act of 2010.
Medicaid Spending on HCBS:
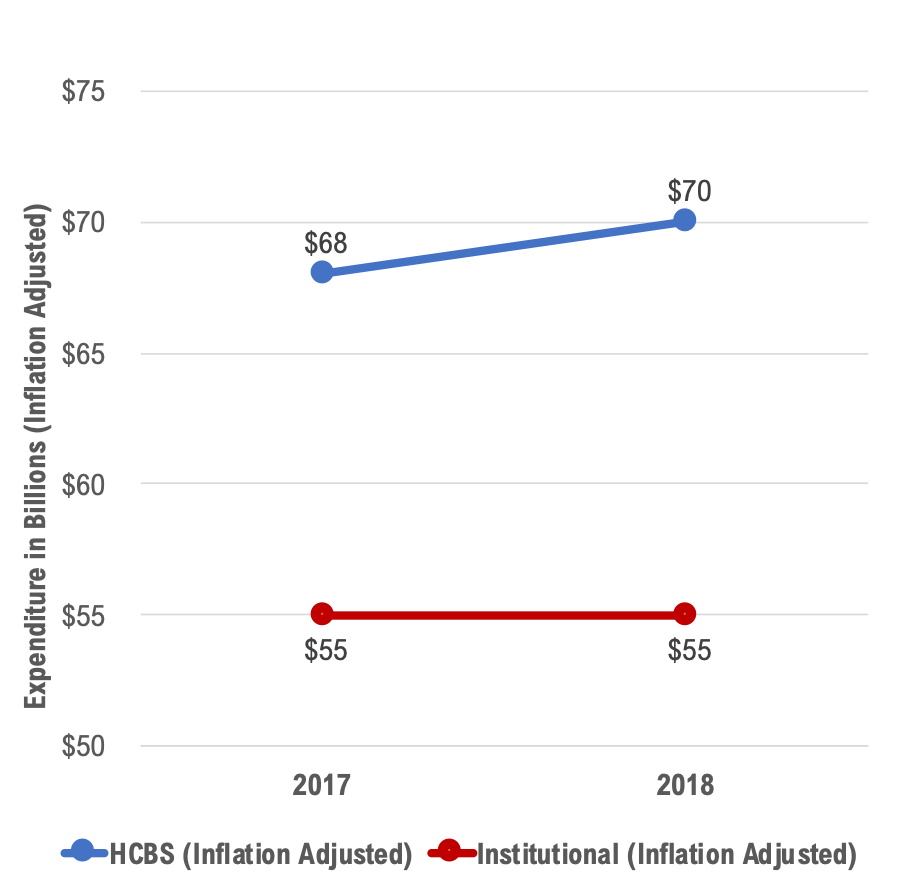
The percentage of HCBS expenditures of total Medicaid LTSS expenditures has steadily increased over the last three decades, but it has slowed in recent years. The U.S. total surpassed the long-standing benchmark of 50 percent of LTSS expenditures in FY 2013 and has remained higher than 50 percent since then, reaching 55.4 percent in FY 2017 and 56.1 percent in FY 2018. In FY 2017, Oregon, Minnesota, and New Mexico spent more than 75 percent of their Medicaid LTSS expenditures on HCBS, and in FY 2018, these same three states, as well as Arizona and Wisconsin, did the same. Florida, Indiana, Louisiana, Mississippi, New Jersey, and Rhode Island all spent less than 40 percent of total Medicaid LTSS expenditures on HCBS in both FY 2017 and 2018.
Source: LTSS Expenditure Report: FY 2017 and FY 2018
Growth of Home and Community-based Services
Medicaid beneficiaries are increasingly receiving LTSS through HCBS. In fiscal year (F.Y.) 2016, Medicaid programs spent approximately $94 billion on HCBS. The federal government and the states spent $116 billion on Medicaid home and community-based services (HCBS) in F.Y. 2020, serving millions of elderly adults and people with disabilities. That is a significant increase in HCBS spending.
Nationally, 3 million people receive HCBS through waivers. Because states can limit enrollment in HCBS waivers, most states report having HCBS waiver waiting lists totaling over 665,000 people nationally. The need for HCBS services will continue to grow in the foreseeable future.
The proportion of Total Medicaid LTSS Spending on Institutional LTSS and HCBS, FYs 2000–2016
Note: LTSS is long-term services and supports. HCBS is home- and community-based services.
Sources: Eiken, S., K. Sredl, B. Burwell, and R. Woodward 2017 and Eiken, S., K. Sredl, B. Burwell, and A. Amos 2018.
The shift in spending from institutional to home- and community-based settings reflects federal and State policies. Referred to as rebalancing, these efforts have been driven by concerns about the high cost of institutional care and to and meet beneficiary preferences to live in the community. They have included the Money Follows the Person (MFP) demonstration program, which provides participating states with grants to assist beneficiaries living in institutions to transition back to the community.
As HCBS grows as the predominant way of delivering LTSS to Medicaid beneficiaries, HCBS policy continues to evolve. Among current developments in HCBS:
States are currently implementing new requirements that HCBS settings must meet to be eligible for Medicaid payment. These requirements ensure that beneficiaries receiving HCBS have adequate choices, their rights are protected, and HCBS is genuinely integrated into the community.
States also are implementing electronic visit verification (EVV) for personal care services. These commonly web-based applications enable personal care services providers to verify their visits to beneficiaries' residences. EVV helps Medicaid programs ensure that authorized personal care services are delivered. EVV can prevent disruptions in beneficiaries' care and protect the Medicaid program against fraud.
Several efforts are underway to develop and test quality measures for HCBS to aid policymakers in overseeing LTSS programs. These efforts, which span both Medicaid fee-for-service and managed LTSS programs, emphasize beneficiary experiences and outcomes.
States take different approaches to managing their HCBS waiver waiting lists, which can influence the length of the waiting list and the wait time before individuals receive HCBS services.
Conclusion:
Without other viable public or private options to finance current and future LTSS needs for people of all ages, Medicaid will remain the significant financing and delivery system for Home and Community-Based Services for millions of Americans. Addressing provider shortages and streamlining access to community-based care that supports functional independence and enhances the quality of life will remain key objectives of states' rebalancing efforts as the need for Medicaid HCBS grows.
COVID-19 has accelerated providing more HCBS instead of Nursing Homes and other institutional services. Proposed additional funding for HCBS will enable states to reduce their HCBS waiver waiting lists and add more people to HCBS.
Home Care Agencies looking for growth and expansion should consider HCBS services as one of the options.
ABOUT CAREVOYANT
CareVoyant is a leading provider of cloud-based integrated enterprise-scale home health care software that can support all home-based services under ONE Software, ONE Patient, and ONE Employee, making it a Single System of Record. We support all home based services, including Home Care, Private Duty Nursing, Private Duty Non-Medical, Home and Community Based Services (HCBS), Home Health, Pediatric Home Care, and Outpatient Therapy at Home.
CareVoyant functions – Intake, Authorization Management, Scheduling, Clinical with Mobile options, eMAR/eTAR, Electronic Visit Verification (EVV), Billing/AR, Secure Messaging, Notification, Reporting, and Dashboards – streamline workflow, meet regulatory requirements, improve quality of care, optimize reimbursement, improve operational efficiency and agency bottom line.
For more information, please visit CareVoyant.com or call us at 1-888-463-6797.
Request for Information
To learn more about CareVoyant Software and how we improve the operational efficiency of Home Healthcare Agencies, contact us: