What Medicaid changes can home care agencies expect after passage of HR1 (OBBBA)? Tips to increase revenue stability.
Introduction
Significant changes to Medicaid will impact home care agencies across the US in 2025 and the years to follow. Although these reforms are intended to improve transparency and service delivery, they present new obstacles for providers of home-based services, especially those heavily reliant on Medicaid reimbursements.
Home care agencies should proactively seek solutions to challenges regulatory upheaval pose. Investing in all-in-one home care software can help agencies tighten up operations and prevent excess revenue leakage. The right home care software will also help agencies meet their compliance metrics efficiently and effectively.
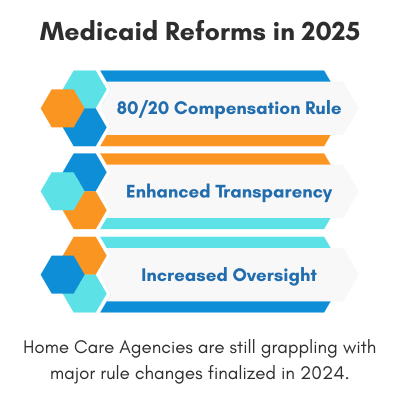
Prior Medicaid Reforms Taking Root in 2025
80/20 Compensation Rule
The Centers for Medicare & Medicaid Services (CMS) finalized a rule in 2024 requiring that at least 80% of Medicaid payments for specific home and community-based services—such as homemaker, home health, and personal care—be allocated directly to compensation for direct care workers. States are required to develop reporting structures by 2028. The payment adequacy threshold takes effect in 2030.
Enhanced Transparency Measures
CMS is implementing new state requirements to report publicly on the percentage of Medicaid payments spent on direct care worker compensation in both institutional and home-and-community-based settings. These measures aim to provide a comprehensive view of Medicaid spending on the direct care workforce.
Increased Oversight on Medicaid Use
Enhanced oversight with the goal of preventing states from using Medicaid funds to subsidize healthcare for ineligible individuals is a top priority for regulators. This increasing oversight is part of a broader effort to increase financial scrutiny and stop improper spending.
New Medicaid Reforms Introduced by HR1 (OBBBA)
Millions of eyes were glued to Washington as they determined the final measures to reform Medicare and Medicaid. The medical industry has been sorely impacted, and home care agencies must organize themselves around these changes sooner rather than later.
Below are some of the most notable Medicaid reforms.
Community Engagement Requirements
By 2026, able-bodied adults between the ages of 19 and 64 will be required to complete 80 hours per month of work, volunteering, and/or attending school to maintain Medicaid eligibility. Certain exemptions for people over the age of 65, or people with certain disabilities, have been worked into the language.
Increased Enrollment and Verification Standards
The bill pauses implementation of certain rules that are meant to streamline enrollment. It also aims to enhance verification standards by requiring address and documentation verification for enrollment.
Increased Frequency of Eligibility Redeterminations
This regulation requires states to reverify Medicaid eligibility every six months, instead of once a year.
Moratorium and Limits on Provider Taxes
The moratorium freezes provider taxes (implemented by some states to increase revenue for Medicaid), and the limits would restrict how provider taxes can be used to finance Medicaid. Effectively, this puts the burden of Medicaid funding further on the state rather than the federal government.
Decreased Medicaid Funding
Though it has its flaws, Medicaid has become the lifeblood of the healthcare industry, and even more so the home care sector. Placing the burden of Medicaid funding on states puts providers at risk, especially in states with a larger rural population. HR1 (OBBBA) decreases Medicaid funding by almost $1 trillion dollars in just a decade by dropping the coverage of approximately 10 million people.
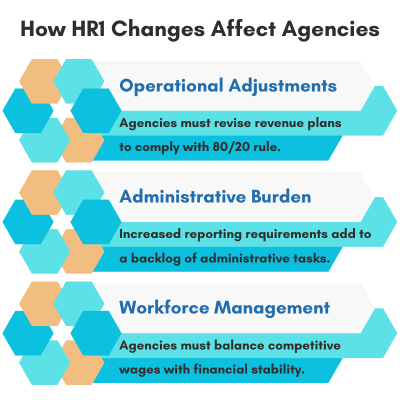
How Medicaid Changes Will Affect Home Care Agencies
Operational Adjustments
Agencies may need to revise their budgeting and payroll processes to comply with the 80/20 compensation rule, which is still in play despite hopes of a moratorium. They must ensure that 80% of Medicaid payments are directed towards direct care worker compensation. Agencies must also have a reliable reporting system in place so they don’t fall out of compliance.
Administrative Burden
Increased reporting requirements are added to the list of administrative tasks. Home care agencies will have to further investigate alternate data management and reporting tools like software for home care agency management.
Workforce Management
Home care agencies might find it challenging to balance competitive wages with overall financial sustainability, especially as dependable Medicaid funding is not guaranteed.
Proactively Preparing for Proposed Changes
By understanding and preparing for Medicaid changes due to HR1, home care agencies can navigate the industry landscape and continue providing essential services to their communities whilst growing their bottom lines. These three tips can help agencies through the uneven terrain:
Review and Adjust Budgets
Ensure that financial plans align with the new compensation requirements ahead of implementation deadlines.
Invest in All-In-One Home Care Software
Invest in software that manages your agency’s operations from Intake all the way through Billing for accurate reporting, increased compliance, and operational efficiency.
Engage with Policy Updates
Stay engaged in ongoing Medicaid reforms to anticipate and adapt to further changes. Reactionary policy adjustments don’t hold up as well as proactively implemented plans.
Conclusion
There has been an onslaught of Medicaid and Medicare changes already – yet more are coming down the pipe. Regulatory upheaval can adversely affect revenue and morale as more administrative tasks are added to the already mile-high pile.
Home care agencies would benefit from making proactive preparations to ensure that all compliance metrics are met and revenue is shored up. Investing in the right software for home care agency management would also reduce administrative burden, increase compliance, and help agencies keep closer tabs on their revenue and bottom line.
Frequently Asked Questions
-
The 80/20 rule requires that 80% of Medicaid payments for specific home and community-based services be spent directly on compensation for direct care workers. It will be enforced by 2030, with reporting frameworks due by 2028.
-
HR1 introduces stricter verification processes, more frequent eligibility redeterminations, and community engagement requirements for able-bodied adults to maintain Medicaid coverage.
-
HR1, also known as the OBBBA, is a legislative reform package that significantly changes Medicaid funding, oversight, and eligibility, directly impacting revenue, compliance, and operations for home care agencies.
-
Beginning in 2026, able-bodied adults aged 19–64 must complete 80 hours per month of work, volunteering, or education to stay eligible for Medicaid, with exceptions for older adults and people with disabilities.
-
Under HR1, Medicaid eligibility will be re-determined every six months, instead of annually, increasing the administrative burden for states and providers alike.
-
Agencies should revise budgets, streamline operations using all-in-one home care software, and focus on meeting compliance and reporting requirements to stabilize revenue.
-
States must develop and implement systems to publicly report how much Medicaid funding is spent on direct care worker compensation by 2028, with compliance thresholds enforced starting in 2030.
-
Yes. HR1 includes a moratorium and restrictions on provider taxes, shifting more financial responsibility for Medicaid to individual states, which may affect provider reimbursement rates.
-
Modern home care software helps agencies manage billing, payroll, compliance reporting, and eligibility verification—critical for maintaining efficiency and reducing revenue leakage under the new Medicaid rules.
-
HR1 is projected to reduce Medicaid funding by nearly $1 trillion over 10 years, with the potential loss of coverage for approximately 10 million individuals.
About CareVoyant
CareVoyant is a leading provider of cloud-based integrated enterprise-scale home health care software that can support all home-based services under ONE Software, ONE Patient, and ONE Employee, making it a Single System of Record. We support all home based services, including Home Care, Private Duty Nursing, Private Duty Non-Medical, Home and Community Based Services (HCBS), Home Health, Pediatric Home Care, and Outpatient Therapy at Home.
CareVoyant functions – Intake, Authorization Management, Scheduling, Clinical with Mobile options, eMAR/eTAR, Electronic Visit Verification (EVV), Billing/AR, Secure Messaging, Notification, Reporting, and Dashboards – streamline workflow, meet regulatory requirements, improve quality of care, optimize reimbursement, improve operational efficiency and agency bottom line.
For more information, please visit CareVoyant.com or call us at 1-888-463-6797.
Request for Information
To learn more about CareVoyant Software and how we improve the operational efficiency of Home Healthcare Agencies, contact us: